Although the SunSmart Campaign runs from December to January, CANSA reminds all South Africans to be SunSmart throughout the year and especially during Summer.
Sunburn can occur within fifteen minutes, and the damage caused is permanent, irreversible and adds up with each exposure to the sun.
Skin cancer is the most common cancer worldwide and SA has one of the highest monitored ultra violet (UV) levels in the world, resulting in one of the highest skin cancer rates globally.
UV radiation is just as dangerous for outdoor labourers, sports people, on the playground or when driving to work, as it is when at the beach or pool. Rays can also reflect off surfaces and cause sunburn when it is overcast.
It’s getting hotter, so be SunSmarter!
Skin Cancer Common In SA
According to the World Health Organisation (WHO), the incidence of both non-melanoma and melanoma skin cancers has been increasing over the past decades, and WHO estimates that a 10 % decrease in ozone levels will result in an additional 300 000 non-melanoma and 4 500 melanoma skin cancer cases globally.
More than 20 000 South Africans were diagnosed with the most common non-melanoma skin cancers (basal cell carcinoma and squamous cell carcinoma) in 2014 and more than 1500 were diagnosed with melanoma.
Fair Skin Tone
People with blonde / red head hair with light skin, freckles and green or blue eyes are more at risk for sunburn and skin damage and need to take extra care to protect their skin.
Albinism and Cancer Risk
People living with the genetic condition Albinism, causing them to be extremely pale, need to take extra special care when outdoors, as they are at greater risk of developing skin cancer, and it’s important that it be detected early when it can be removed by surgery. They need to wear protective clothing and sunglasses to protect their sensitive eyes. It’s also important that they seek employment in a shaded environment and go for regular examinations to monitor for skin cancer. Sunscreen is available through prescription from the Department of Dermatology at public hospitals. Read more about Albinism and cancer risk…
People with Darker Skin also at Risk

Nikki Seboni, skin cancer Survivor…
It is important to take note of the fact that everyone, regardless of racial or ethnic group, is at risk of getting skin cancer. Although people with darker skins are less susceptible, because their skin contains more natural melanin, that protects against sun damage, everyone is at risk from the harsh African sun.
Although people with darker skins are at a lower risk of melanoma than lighter skinned groups, the majority of basal cell carcinomas, in people with darker skins, occur in sun-exposed skin, indicating that sun protection is paramount, regardless of pigment. ¹
In darker skins, 70 % of melanomas have been reported to be on the lower limb, with 90% of those being below the ankle. The most common subtype, acral lentiginous melanoma, appears on the palms of the hands and soles of the feet. ²
Nikki Seboni believed that skin cancer was a white person’s disease, until she was diagnosed at the age of 25 years. Read more…
¹ Gloster HM Jr, Neal K. Skin cancer in skin of color. J Am Acad Dermatol 2006;55:741-60
² Hudson DA, Krige JE. Melanoma in black South Africans. J Am Coll Surg 1995;180:65-71
Types Skin Cancer
There are two main categories of skin cancer, namely, melanoma and non-melanoma.
Melanoma, is less common than other skin cancers, but it is the most dangerous. It is of special importance to note that excessive ultraviolet (UV) radiation received as a child, increases the risk of melanoma later in life. Melanoma is linked with short, sharp bursts of over-exposure, so even one incident of bad sunburn, especially in childhood, can later on in life, trigger damage and develop into a melanoma.

Former Mrs SA Nicole Capper, melanoma skin cancer Survivor
Former Mrs South Africa, Nicole Capper, a skin cancer Survivor says, “As a cancer Survivor sun protection is a massive focus for me. Being diagnosed with malignant melanoma at 25 rocked my world, but I was lucky to have caught it early enough. We’re so aware of other potential health concerns and we make sure we visit specialists annually for other standard check-ups, and yet our skin is neglected for the most part, often until it’s too late. Sunscreen is always healthy. And regular dermatologist appointments should be mandatory. We owe it to our families and communities to stay healthy, and our skin is no exception.”
Non-melanoma skin cancers mainly comprise Basal Cell Carcinoma and Squamous Cell Carcinoma. Of these, Basal Cell Carcinoma is the most common and the least dangerous. These cancers are linked to long term exposure to the sun, for example people with professional sports careers or outside occupations. If left untreated, these can lead to disfigurement, or the loss of an eye, nose or ear, so early detection is important.
Squamous Cell Carcinoma (SCC) is most frequently seen on sun-exposed areas of the body such as the head, neck and back of the hands. Although women frequently get SCC on their lower legs, it is possible to get SCC on any part of the body, including the inside of the mouth, lips and genitals. People who use tanning beds have a much higher risk of getting SCC – they also tend to get SCC earlier in life.
Other skin cancers include:
Kaposi Sarcoma | Merkel Cell Carcinoma | Sebaceous Gland Carcinoma
The following conditions can give rise to cancer or be mistaken as cancer:
- Spitz Naevi (usually present in toddlers and children), can mistakenly be thought to be Malignant Melanoma because of the close resemblance…
- Actinic Cheilitis and Actinic Keratosis – are pre-cancerous conditions that can lead to Squamous Cell Carcinoma
- Bowen’s Disease – is a pre-cancerous condition that can lead to Squamous Cell Carcinoma
- Gorlin-Goltz Syndrome, is an inherited medical condition involving defects within multiple body systems such as the skin, nervous system, eyes, endocrine system, and bones. People with this syndrome are particularly prone to developing a common form of non-melanoma skin cancer, e.g. Basal Cell Carcinoma
- Solar Elastosis – is a pre-cursor to Squamous Cell Carcinoma
- Xeroderma Pigmentosum (XP) – an inherited condition characterised by an extreme sensitivity to ultraviolet (UV) rays from sunlight. Most people with XP develop multiple skin cancers during their lifetime.
Myths
- The sun is only dangerous in summer or on a hot day
- Sunscreen will protect me completely from the harmful effects of the sun’s rays
- One or two cases of sunburn won’t result in skin cancer
- People with darker skins are not at risk for getting skin cancer
- Sunbeds are a safer alternate to obtain a tan – find out why sunbeds should be banned…
- Infographic: SunSmart Truth vs Myths
With credit to Thomas Leveritt (original YouTube video) – An ultraviolet camera can show not-yet visible changes to your skin…
The Truth About Tanning
Sunbeds
People who think that indoor tanning or sunbeds are a safer option are mistaken. There is no such thing as a healthy tan, which in fact indicates skin damage. First use of sunbeds before age 35, increases the risk of developing melanoma by 59%. In 2009 sunbeds and tanning booths were officially classified as cancer causing agents by the International Agency for Research on Cancer (IARC). People who use tanning beds also have a much higher risk of getting Squamous Cell Carcinoma (SCC) – they also tend to get SCC earlier in life. Read more about the dangers of sunbeds…

Julie George melanoma Survivor
Julie George, melanoma Survivor states: “I think in the back of my mind I knew sunbeds were dangerous, but I never knew just how dangerous. I was completely ignorant of the nature of melanoma too. I wish I could have had a glimpse into the future back then, a real understanding of the dangers. I still find people today who don’t take it seriously. I think as I had, they have the ‘it won’t happen to me mind set.’ I am hoping my story will convince people that this is a very real, life threatening risk.”
Sunless or Self-Tanning
There is no such thing as a healthy tan – even a sunless tan…
In recent years there has been a considerable increase in the use of sunless and self-tanning products such as sprays, mousses, gels, pills, nasal sprays & injections called Melanotan 1 and 11.
Melanotan 11 has serious side effects, and may induce melanoma. CANSA warns against this product. Read our Warning Against Melanotan-II…
Sunless tanning, also known as UV-free tanning, self-tanning, spray-tanning (when something is applied topically) or fake-tanning – refers to the application of chemicals to the skin or making use of chemicals that are taken by mouth or per injection, to produce an effect similar in appearance to a suntan. The browning effect usually occurs within a few hours. The effect is temporary – the colour fades in 7-10 days as the skin naturally sloughs off.
Sunless tanning products include:
- Bronzing powder
- Spray bronzers
- Stick bronzers
- Tanning wipes
- Tanning tablets
- Tanning capsules
- Tanning injections
- Tanning nasal spray
- Sunless tanning lotion
None of these is safe!
- Although some self-tanning products contain sunscreen, it offers minimal ultraviolet radiation protection. It does not provide protection from the ultraviolet rays of the sun and CANSA strongly discourages individuals to use any form of tanning product.
- Topical sunless tanning products that contain Dihydroxyacetone (DHA), prevent the formation of Vitamin D in the skin when exposed to the sun.
Read our Sunless Tanning Position Statement & Fact Sheet
How to Lower your Skin Cancer Risk:
1. Do a Monthly “Spot the Spot” Check Up:
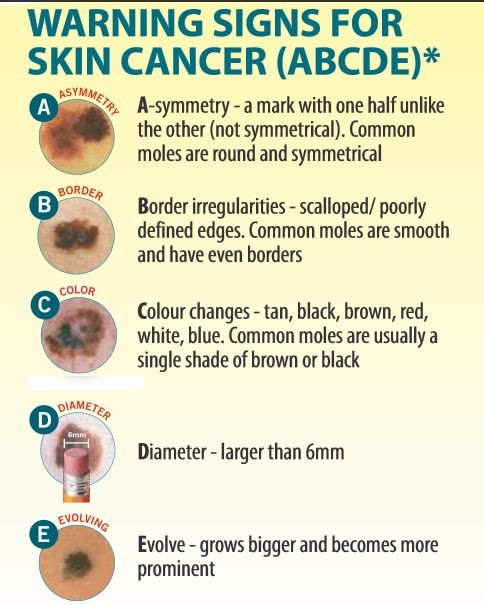
Always seek medical advice as soon as possible when concerned about a particular spot on your skin. Check your skin carefully every month and ask a family member or friend to examine your back and the top of your head. If you notice any of these warning signs, see a doctor or dermatologist immediately – follow the A B C D E Warning Signs:
CANSA has partnered with Miiskin, a free user-friendly app for monitoring changes on your skin, although it doesn’t replace a doctor’s visit and isn’t a diagnostic tool. Any suspicious moles or abnormalities should be checked out by a dermatologist or medical professional. It’s another way to encourage people to be aware of skin changes and to monitor them. Extra functionalities can be accessed through a subscription that comes with a 30-day free trial and if consumers take this up, Miiskin donates 15% of subscriptions to CANSA to assist in implementing our risk reduction and support work.
2. Get Screened at Your Local CANSA Care Centre
- Go to your local CANSA Care Centre for screening with our FotoFinder Dermoscope machine – be sure to make an appointment as the machines ‘roam’ between Care Centres.
- If you are concerned re symptoms, please do not wait – contact your Care Centre, doctor or dermatologist immediately.
3. Avoid the Following
- Stay out of the sun between 10am and 3pm – stay under the shade of trees or an umbrella as much as possible
- Avoid sunbeds & sunlamps
Tips: Sunscreen & Protective Garments
With credit to TED-Ed. Original video at Why do we have to wear sunscreen – Kevin P. Boyd
Old CANSA SunSmart Seal logo, being phased out…
1. Use an Effective Sunscreen
- We have raised our Seal of Recognition standards & requirements for sunscreens. In addition to current SA standards, as of 1 April 2013, sunscreens bearing our Seal need to comply with the European Colipa Standards.
- Our CANSA Seal of Recognition logo (CSOR) appears on approved sunscreen products and is a guarantee that the manufacturers of these UV protective products have complied with CANSA’s strict set of criteria – see logo below.
- See list of CANSA’s SunSmart Sunscreen Partners…
- Be sure to use a sunscreen with an SPF of between 20 and 50 & 30 and 50 for fair to very fair skin.
- Products usually expire two years after manufacture – don’t use a product that has been opened and used after a year has passed.

Old CANSA SunSmart Seal logo, being phased out…

New Smart Choice Seal logo for SunSmart products / gear
2. Apply Sunscreen Correctly
- It’s important to know the best SPF for your skin-type
- Always apply sunscreen 20 minutes before you go outside and re-apply at least every two hours, after towel drying, perspiring or swimming.
3. Wear Protective Clothing
- Wear sunglasses with a UV protection rating of UV400
- Wear protective clothing & swimsuits and thickly-woven fabric hats with wide brims – avoid caps where the neck & ears are exposed
- Buy SunSmart garments & apparel… – look out for CANSA’s swing tags (below) & SunSmart Choice logo (top right) on clothing, hats & summer fun accessories.
Educate & Protect Children
Our youth should take special precaution when spending time in the sun – two blistering burns before the age of 18, can dramatically increase the risk of getting skin cancer later in life.
Parents and schools need to play an increasingly important role in educating our youth re being SunSmart. Unfortunately a recent study shows that most schools are not SunSmart. Read more…
Babies younger than 1 year should never be exposed to direct sunlight.
- Being SunSmart with Infants, Toddlers & Children Fact Sheet
- SunSmart Radio Spots featuring UV Rays & Villains, Sunny & Brand for children | parents | educators – listen to this with your children or students: English | Afrikaans





