Fact Sheet on Climate Change, Heatwaves, and the Incidence of Skin Cancer
Introduction
The World Meteorological Organisation (WMO) describes the build-up of greenhouse gases in the atmosphere as a major cause of climate change. It states that “… the growing use of energy and expansion of the global economy are factors resulting in the build-up of greenhouse gases in the atmosphere which alters the radiative balance of the atmosphere. The net effect of this is warming of the Earth’s surface as well as the lower atmosphere because greenhouse gases absorb some of the earth’s outgoing heat radiation and reradiate it back towards the surface.” (United Nations Framework Convention on Climate Change).
[Picture Credit: UNFCCC]
Climate Change
The United Nations Framework Convention on Climate change (UNFCCC) defines climate change as follows: “’Climate change’ means a change of climate which is attributed directly or indirectly to human activity that alters the composition of the global atmosphere and which is in addition to natural climate variability observed over comparable time periods.” (United Nations Framework Convention on Climate Change).
According to the South African Weather Service, “Climate change is the natural cycle through which the earth and its atmosphere are going to accommodate the change in the amount of energy received from the sun. The climate goes through warm and cold periods, taking hundreds of years to complete one cycle. Changes in temperature also influence the rainfall, but the biosphere is able to adapt to a changing climate if these changes take place over centuries. Unfortunately, human intervention is currently causing the climate to change too fast. (Climate models predict that the mean air temperature over South Africa will increase by an estimated 2°C over the next century.)” (South African Weather Service).
Parker, E.R. 2020.
Background: Climate change is broadly affecting human health, with grave concern that continued warming of the earth’s atmosphere will result is serious harm. Since the mid-20th century, skin cancer incidence rates have risen at an alarming rate worldwide.
Objective: This review examines the relationship between climate change and cutaneous carcinogenesis.
Methods: A literature review used the National Institutes of Health databases (PubMed and Medline), the Surveillance, Epidemiology, and End Results and International Agency for Research on Cancer registries, and published reports by federal and international agencies and consortia, including the Australian Institute of Health and Welfare, Climate and Clean Air Coalition, U.S. Environmental Protection Agency, Intergovernmental Panel on Climate Change, National Aeronautics and Space Administration, National Oceanic and Atmospheric Administration, United Nations Environment Programme, World Health Organization, and World Meteorological Organization.
Results: Skin cancer risk is determined by multiple factors, with exposure to ultraviolet radiation being the most important. Strong circumstantial evidence supports the hypothesis that factors related to climate change, including stratospheric ozone depletion, global warming, and ambient air pollution, have likely contributed to the increasing incidence of cutaneous malignancy globally and will continue to impose a negative on influence skin cancer incidence for many decades to come.
Conclusion: Because much of the data are based on animal studies and computer simulations, establishing a direct and definitive link remains challenging. More epidemiologic studies are needed to prove causality in skin cancer, but the evidence for overall harm to human health as a direct result of climate change is clear. Global action to mitigate these negative impacts to humans and the environment is imperative.
Silva, G.S. & Rosenbach, M. 2020.
“Anthropogenic global climate change is a well-documented phenomenon that has led to average global temperatures climbing to approximately 1 °C above preindustrial (1850-1900) levels, with even higher regional deviations in some areas and significantly increased average warming in densely populated urban centers. In 2018, the United Nations Intergovernmental Panel on Climate Change set a threshold of 1.5 °C of average warming (above the preindustrial baseline), beyond which our planet will become significantly less hospitable to human life. However, adverse human health impacts are already occurring due to current levels of global climate change, as summarized by publications such as The Lancet’s annual “Countdown on Health and Climate Change,” initiated in 2016. The human health impacts of climate change are truly cross-disciplinary, with nearly every medical specialty either already facing or set to face effects. The field of dermatology is not immune to these risks. This special issue of the International Journal of Women’s Dermatology is dedicated to the cross section of dermatology and climate change. This initial article will serve as an overview to introduce readers to the topic and to lay the groundwork for the rest of the issue. We are delighted to work with the Women’s Dermatological Society and welcome their support for this dedicated issue. Herein, you will read from up-and-coming stars in the field and established experts, including articles on the following key areas: infectious diseases, environmentally friendly office practices, sunscreens and the environment, refugee health, heat-related illness, the effect of air pollution on the skin, the impact of climate change on pediatric dermatology, implications for skin cancer, and skin issues related to flooding and extreme weather events.”
Moreira, R.S., Bicker, J., Musicco, F., Persichetti, A. & Pereira, A.M.P.T. 2020.
“Immunotherapy with immune checkpoint inhibitors, such as anti-PD-1 drugs, is an area in increasing development for its efficacy and advantages in the treatment of advanced metastatic melanoma. In fact, immunotherapy has been the target of several and recent studies in different types of cancer, namely in melanoma, a globally growing threat. Contributing to the increasing incidence of this cancer is climate change, particularly global warming of the past century, which has increased the tendency to spend more time outdoors and, consequently, exposure to sunlight and ultraviolet radiation. Among the most relevant risk factors for melanoma is the increase in ultraviolet radiation due to ozone layer depletion, one of the main factors responsible for the incidence of new cases. Anti-PD-1 agents like Nivolumab and Pembrolizumab allow a more effective treatment, enhancing the duration of the responses to therapy and prolonging the survival of the patient. However, recent studies about safety and tolerability have stated that, although these drugs present less adverse effects and toxicity, they may lead to specific autoimmune-mediated adverse events. Overall, immunotherapy with anti-PD-1 agents represents a highly promising area in the treatment of some types of cancer such as melanoma.”
Wright, C.Y., du Preez, D.J., Millar, D.A. & Norval, M. 2020. The epidemiology of skin cancer and public health strategies for its prevention in Southern Africa. Int J Environ Res Public Health. 2020 Feb 6;17(3):1017. doi: 10.3390/ijerph17031017.
“Skin cancer is a non-communicable disease that has been underexplored in Africa, including Southern Africa. Exposure to solar ultraviolet radiation (UVR) is an important, potentially modifiable risk factor for skin cancer. The countries which comprise Southern Africa are Botswana, Lesotho, Namibia, South Africa, and Swaziland. They differ in population size and composition and experience different levels of solar UVR. Here, the epidemiology and prevalence of skin cancer in Southern African countries are outlined. Information is provided on skin cancer prevention campaigns in these countries, and evidence sought to support recommendations for skin cancer prevention, especially for people with fair skin, or oculocutaneous albinism or HIV-AIDS who are at the greatest risk. Consideration is given to the possible impacts of climate change on skin cancer in Southern Africa and the need for adaptation and human behavioural change is emphasized.”
Placentini, R.D., Della Ceca, L.S. & Ipiña, A. 2018.
“Climate change is affecting both the environment and human behaviour. One significant impact is related to health, as detailed in the IPCC 2014 report. In the present work, and as a contribution to this commemorative special issue to Prof. Dr Jan van der Leun, we present the results of the squamous (SCC) and basal-cell carcinoma (BCC) incidence change in relation to the ambient temperature increase. This increase is produced by global warming, mainly induced by anthropogenic atmospheric emissions of greenhouse gases. We have broadened a previous study conducted by van der Leun et al. (Photochem. Photobiol. Sci., 2008, 7, 730-733), by analysing the effective carcinogenicity of UV dose, for the period 2000-2200 and four climate change scenarios (called RCP2.6, RCP4.5, RCP6.0 and RCP8.5). The corresponding percentage increases of the incidence of SCC for 2100 are 5.8, 10.4, 13.8 and 21.4%, and for 2200 they are 4.3, 12.1, 19.0 and 40.5%. In a similar way, the percentage increases of the incidence of BCC for 2100 are 2.8, 4.9, 6.5 and 9.9% and for 2200 they are 2.0, 5.8, 8.9 and 18.2%. We report the SCC and BCC percentage effective incidence results as a function of time, for the whole 21st century and we extended the analysis to the 22nd century, since people possibly affected (like the Z and T generations, born at the beginning of this century) will have a life expectancy extending up to the final decades of the present century and even to the first ones of the next century.”
Heatwaves
A heatwave normally refers to a period of prolonged abnormally high surface temperatures relative to those normally expected. Heat waves may span several days to several weeks and are significant causes of weather-related mortality, affecting developed and developing countries alike. Although there is no formal, standardised definition of a heatwave, the World Meteorological Organization, defines it as “five or more consecutive days during which the daily maximum temperature surpasses the average maximum temperature by 5 °C or more.” (Encyclopaedia Britannica).
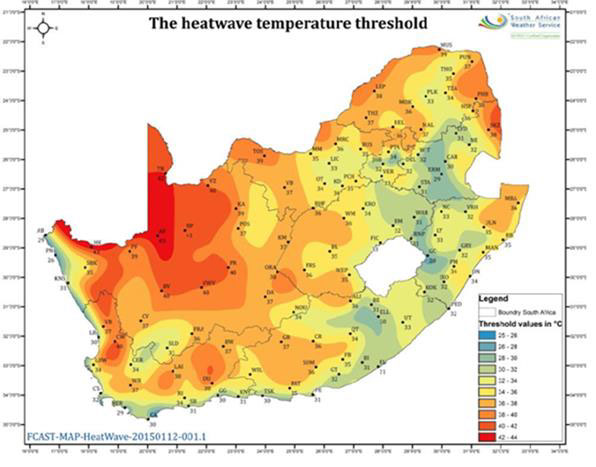
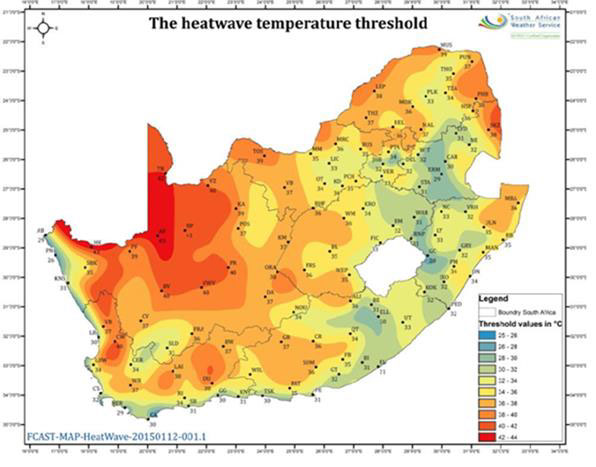
[Picture Credit: SA Heatwave Threshold Map]
There is a specific criterion that the South African Weather Service applies to each town or city, in order to determine whether heat wave conditions are met or not.
The criterion reads as follows: “If the maximum temperature at a particular town is expected to meet or exceed 5 degrees C above the average maximum temperature of “the hottest month” for that particular place, as well as persisting in that mode for 3 days or more, then a heat wave may be declared. For ease of use by SAWS meteorologists, a detailed map of the ‘heat wave threshold’ has been compiled (see figure on right), using the latest climatological data to hand. This threshold is thus the maximum temperature which needs to be met or exceeded, for a heat wave to occur.” (South African Weather Service).
Changing Climatic Patterns
According to the World Health Organization, 2018 (WHO), the world has warmed by approximately 0.85oC over the last 130 years and each of the last 3 decades has been successively warmer than any preceding decade since 1850.
WHO further mentions that:
• Sea levels are rising
• Glaciers are melting
• Precipitation patterns are changing
• Extreme weather events are becoming more intense and frequent
• Climate change is affecting social and environmental determinants of
▪ health
▪ clean air
▪ safe drinking water
▪ sufficient food
▪ secure shelter
Key Facts
• Climate change affects the social and environmental determinants of health – clean air, safe drinking water, sufficient food and secure shelter.
• Between 2030 and 2050, climate change is expected to cause approximately 250 000 additional deaths per year, from malnutrition, malaria, diarrhoea and heat stress.
• The direct damage costs to health (i.e. excluding costs in health-determining sectors such as agriculture and water and sanitation), is estimated to be between USD 2-4 billion/year by 2030.
• Areas with weak health infrastructure – mostly in developing countries – will be the least able to cope without assistance to prepare and respond.
• Reducing emissions of greenhouse gases through better transport, food and energy-use choices can result in improved health, particularly through reduced air pollution. (World Health Organization, 2018)
Shezi, B., Mathee, A., Siziba, W., Street, R.A., Naicker, N., Kunene, Z. & Wright, C.Y. 2019.
“The Intergovernmental Panel on Climate Change (IPCC), the World Health Organization and other international institutions have indicated that climate change will exacerbate or redistribute current environmental health risks. Vulnerable population groups in South Africa, especially those living in poverty, children, women, the elderly and people with pre-existing diseases, are susceptible to health threats resulting from climate change, such as increasing temperature, floods and droughts. Little is known about the coping capacities of vulnerable sub-populations with respect to these climate change-related environmental effects. Environmental Health Practitioners (EHPs) play an important role in local implementation of adaptation strategies, particularly in communities with vulnerable populations. Equally so, climate change adaptation tends often correspond more closely to environmental health practice at a local rather than global level.
“IPCC defines Southern Africa as a region likely to experience an increase in temperature that exceeds the global average. In South Africa the average annual temperatures are reported to have increased by 1.5 °C times the observed 0.65 °C over the past five decades. The frequency in extreme rainfalls has also increased. It is predicted that interior regions of South Africa will warm by a further ~ 3–4 °C by 2100.”
Frumkin, H. & Haines, A. 2019.
“Multiple global environmental changes (GECs) now under way, including climate change, biodiversity loss, freshwater depletion, tropical deforestation, overexploitation of fisheries, ocean acidification, and soil degradation, have substantial, but still imperfectly understood, implications for human health. Noncommunicable diseases (NCDs) make a major contribution to the global burden of disease. Many of the driving forces responsible for GEC also influence NCD risk through a range of mechanisms. The research provides an overview of pathways linking GEC and NCDs, focusing on five pathways: (a) energy, air pollution, and climate change; (b) urbanization; (c) food, nutrition, and agriculture; (d) the deposition of persistent chemicals in the environment; and (e) biodiversity loss.”
Climate and an Increase in the Incidence of Skin Cancer
Weather pattern changes have accelerated rapidly during the past half century. International focus has concentrated on environmental and economic consequences of these changes while very little attention has been paid to the effects on human diseases such as skin cancer. There is scientific evidence of the association between ultraviolet (UV) radiation and the development of malignant skin diseases. (Barath & Turner, 2009).
Van der Leun, J.C., Piacentini, R.D. & de Gruijl, F.R. 2008.
“As part of an inventory of potential interactions between effects of ozone depletion and climate change, a possible effect of ambient temperature on sun-induced skin cancers was suggested. Mouse experiments had shown that increased room temperature enhanced ultraviolet (UV) radiation-induced carcinogenesis; the effective UV dose was increased by 3-7% per degrees C. The present investigation was aimed at studying a possible temperature effect on human skin cancer. Existing data on the incidence of human skin cancer were analyzed, as available from two special surveys of non-melanoma skin cancer in the United States. The incidence of non-melanoma skin cancer in the ten regions surveyed not only correlated significantly with the ambient UV dose but also with the average daily maximum temperature in summer. For squamous cell carcinoma the incidence was higher by 5.5% (SE 1.6%) per degrees C and for basal cell carcinoma by 2.9% (SE 1.4%) per degrees C. These values correspond to an increase of the effective UV dose by about 2% per degrees C. Although the precise nature of this correlation with temperature requires further studies, it can be concluded that the temperature rises coming with climate change can indeed amplify the induction of non-melanoma skin cancers by UV radiation in human populations.”
Bharath, A.K. & Turner, R.J. 2009.
“… ozone depletion and climate change are separate entities which are intricately linked. They both have the potential to increase the incidence of skin cancer through different means. Over the last 30 years ozone depletion has received much of the attention, leading to the Montreal Protocol; heralded by Kofi Annan as ‘perhaps the single most successful international agreement to date’. Ozone depletion has led to an increase in skin cancers and worryingly this is still rising. The depletion will however peak and then the ozone layer will begin to repair itself. Focus must now shift towards analysing the social and behavioural changes that will come about through climate change. Warmer, drier weather in the UK is likely to encourage people to spend more time outdoors and increase their exposure to UVR. The consequence will be an increase in the incidence of skin cancer brought about by behavioural change rather than environmental change. The world has had 30 years of public health initiatives and awareness campaigns. These must be heeded and acted upon now to protect the public from this preventable threat.”
Australian Health Promotion Association. 2011
“Australian data shows that with higher temperatures, adults spend more time outdoors, are less likely to wear covering clothing and more likely to be sunburnt. Hence, rising temperatures can be expected to result in increases in sun exposure, sunburn and correspondingly, skin cancer risk.”
Cancer Council Australia. 2016.
“According to the CSIRO and the Bureau of Meteorology, mean temperatures within Australia are projected to rise by 0.6 to 1.5°C by 2030 compared with the climate of 1980 to 1999. Warmer temperatures may result in Australians increasing their sun exposure and wearing less covering clothing, thereby increasing their risk of skin cancer. However, very high temperatures may instead prompt behaviours to avoid sun exposure, and therefore ‘there is considerable uncertainty in modeling future human behaviour in response to climate change’. There is weak animal model evidence that higher ambient temperatures may increase the skin cancer-effective UV dose by a few percent per Celsius, which would result in more skin cancers for the same level of UV radiation.”
European Climate Adaptation Platform. 2016
“It is predicted that by 2050-2080 the local climate will be 2 to 3 °C warmer than now, both in winter and summer, and that there will be longer periods of hot and dry weather in spring and summer. Overall, levels of precipitation will be similar to now, but more concentrated in the winter months. In addition, it is predicted that extreme weather events will become more frequent, including heatwaves, storms, heavy rainfall, and cold spells. These changes will occur over the medium term, and are within the time frame of planning and development. Due to the increase in temperatures, it is also likely that individual’s exposure to UV radiation will increase, and therefore the risk of developing skin cancer.”
Edith Cowan University, Australia. 2016
“Exposure to ultra-violet (UV) light has long been established as the main cause of skin cancer. Research from Edith Cowan University (ECU) has revealed that temperature may also play a major role, with a difference of just two degrees potentially significantly increasing the risk of developing the skin cancer.
Researchers from ECU’s Melanoma Research Group exposed two samples of human skin cells to UV light, keeping one sample at 37°C and the other at 39°C. When they analysed the skin cells they found that those exposed to the 39°C temperature had significantly more DNA damage, a major risk factor for developing skin cancer.
“Lead researcher Dr Leslie Calapre said the higher temperature appeared to inhibit the tumour-supressing protein p53 in skin cells. “The p53 protein is responsible for mediating repair and/or the death of cells that harbour DNA damage. Suppression of this protein after exposure to UV and heat allows for the survival of damaged cells and thus potentially increases the risk that a cancerous tumour will develop,” she said.”
Calapre, L., Gray, E.S., Kurdykowski, S., David, A., Hart, P., Descargues, P. & Ziman, M. 2016.
“Exposure to ultra-violet (UV) light has long been established as the main cause of skin cancer. Lead Researcher, Dr Calapre, from ECU’s Melanoma Research Group states that the findings of their research were of particular significance to workers in industries that are required to work outside and exposed to high levels of heat. Our research shows that in industries like mining, construction and agriculture operating in areas that regularly see high temperatures, should protect workers from skin cancer and not just minimising their UV exposure, but also doing things to reduce the levels of ambient heat for workers.
“Things like allowing workers to take regular breaks in air-conditioned areas on hot days, doing work in the shade wherever possible and making sure that protective clothing allows good air flow could all be ways of potentially minimising risk.”
Piacentini, R.D., Ceca, L.S.D. & Ipina, A. 2018. Climate change and its relationship with non-melanoma skin cancers. Photochemical & Photobiological Siences. 2018. “Climate change is affecting both the environment and human behaviour. One significant impact is related to health, as detailed in the IPCC 2014 report. In the present work, and as a contribution to this commemorative special issue to Prof. Dr Jan van der Leun, we present the results of the squamous (SCC) and basal-cell carcinoma (BCC) incidence change in relation to the ambient temperature increase. This increase is produced by global warming, mainly induced by anthropogenic atmospheric emissions of greenhouse gases. We have broadened a previous study conducted by van der Leun et al. (Photochem. Photobiol. Sci., 2008, 7, 730–733), by analysing the effective carcinogenicity of UV dose, for the period 2000–2200 and four climate change scenarios (called RCP2.6, RCP4.5, RCP6.0 and RCP8.5). The corresponding percentage increases of the incidence of SCC for 2100 are 5.8, 10.4, 13.8 and 21.4%, and for 2200 they are 4.3, 12.1, 19.0 and 40.5%. In a similar way, the percentage increases of the incidence of BCC for 2100 are 2.8, 4.9, 6.5 and 9.9% and for 2200 they are 2.0, 5.8, 8.9 and 18.2%. We report the SCC and BCC percentage effective incidence results as a function of time, for the whole 21st century and we extended the analysis to the 22nd century, since people possibly affected (like the Z and T generations, born at the beginning of this century) will have a life expectancy extending up to the final decades of the present century and even to the first ones of the next century.”
The Global Climate and Health Alliance. 2019.
“As the findings of the Intergovernmental Panel on Climate Change, and a recent report by the Global Climate and Health Alliance show, Australia is in no way immune to the health impacts of climate change. One such impact can be seen with the increasing risk of skin cancer. Australia already has the highest rate of skin cancer in the world – astonishingly, 2/3 of all Australians will have been diagnosed with some form of skin cancer by the time they are 70 – and the incidence is expected to continually rise in correlation with rising ambient temperatures.”
Key Findings of Research:
Ambient temperature of above 27oC and particularly 29oC and above contributes to DNA damage in skin cells increasing the risk for various skin cancers:
• Ambient temperature significantly correlates with ambient UV dose
• Ozone depletion has led to an increase in skin cancers
• Behavioural changes contributes to an increase in skin cancer
• A rise in environmental temperature coming with climate change can amplify the induction of non-melanoma skin cancers by UV radiation in human populations
• Warmer temperatures may result in individuals increasing their sun exposure and wearing less covering clothing resulting in an increase in skin cancer
• Increased environmental temperatures above 37oC results in DNA damage of skin cells
• Incidence of skin cancer is expected to continually rise in correlation with rising ambient temperatures
• Industries like mining, construction and agriculture operating in areas that regularly see high temperatures, should actively protect their workers from increased environmental temperature so as to reduce the risk of DNA damage in skin cells
Medical Disclaimer
This Fact Sheet is intended to provide general information only and, as such, should not be considered as a substitute for advice, medically or otherwise, covering any specific situation. Users should seek appropriate advice before taking or refraining from taking any action in reliance on any information contained in this Fact Sheet. So far as permissible by law, the Cancer Association of South Africa (CANSA) does not accept any liability to any person (or his/her dependants/estate/heirs) relating to the use of any information contained in this Fact Sheet.
Whilst the Cancer Association of South Africa (CANSA) has taken every precaution in compiling this Fact Sheet, neither it, nor any contributor(s) to this Fact Sheet can be held responsible for any action (or the lack thereof) taken by any person or organisation wherever they shall be based, as a result, direct or otherwise, of information contained in, or accessed through, this Fact Sheet.
Sources and References Consulted and/or Utilised
Read More
cansa.org.za/be-sunsmart/