What is Tuberculosis?
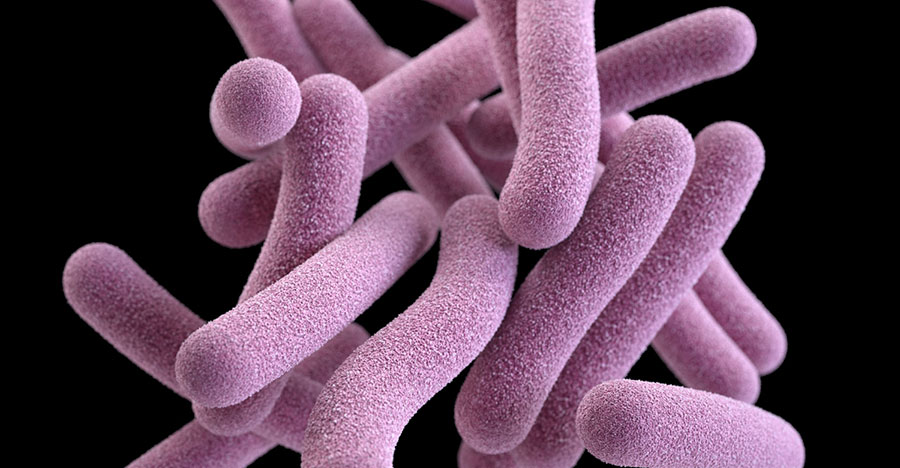
Tuberculosis — or TB, as it’s commonly called — is a contagious infection that usually attacks your lungs. It can spread to other parts of your body, like your brain and spine. A type of bacteria called Mycobacterium tuberculosis causes it.
In the early 20th century, TB was a leading cause of death in the United States. Today, most cases are cured with antibiotics. But it takes a long time. You have to take meds for at least 6 to 9 months.
In the 20th century, TB was a leading cause of death in the United States. Today, most cases are cured with antibiotics. But it takes a long time. You have to take meds for at least 6 to 9 months.
Tuberculosis Types
A TB infection doesn’t mean you’ll get sick. There are two forms of the disease:
Latent TB. You have the germs in your body, but your immune system stops them from spreading. That means you don’t have any symptoms and you’re not contagious. But the infection is still alive in your body and can one day become active. If you’re at high risk for re-activation — for instance, you have HIV, your primary infection was in the past 2 years, your chest X-ray is abnormal, or your immune system is compromised — your doctor will treat you with antibiotics to lower the risk for developing active TB.
Active TB. This means the germs multiply and can make you sick. You can spread the disease to others. Ninety percent of adult cases of active TB are from the reactivation of a latent TB infection.
Tuberculosis Signs and Symptoms
There aren’t any for latent TB. You’ll need to get a skin or blood test to find out whether you have it.
There are usually signs if you have active TB disease. They include:
- A cough that lasts more than 3 weeks
- Chest pain
- Coughing up blood
- Feeling tired all the time
- Night sweats
- Chills
- Fever
- Loss of appetite
- Weight loss
If you have any of these symptoms, see your doctor to get tested. Get medical help right away if you have chest pain.
Tuberculosis Causes and How TB Is Spread
Tuberculosis is caused by bacteria that spread through the air, just like a cold or the flu. When someone who has it coughs, sneezes, talks, laughs, or sings, tiny droplets that contain the germs are released. If you breathe in these germs, you can get it.
TB can spread from person to person, but it isn’t easy to catch. You usually have to spend a lot of time around someone who has a lot of bacilli in their lungs. You’re most likely to catch it from co-workers, friends, and family members.
Tuberculosis germs don’t thrive on surfaces. You can’t get the disease from shaking hands with someone who has it or by sharing their food or drink.
Tuberculosis Diagnosis
There are two common tests for tuberculosis, but they don’t tell you whether you have latent or active TB:
- Skin test. This is also known as the Mantoux tuberculin skin test. A health care worker injects a small amount of fluid into the skin of your lower arm. After 2 or 3 days, they’ll check for swelling in your arm to determine your results. If your results are positive, you probably have been infected with TB bacteria. But the results can be false positive. If you’ve gotten a tuberculosis vaccine called bacillus Calmette-Guerin (BCG), the test could say you have TB when you really don’t. The results can also be false negative, saying that you don’t have TB when you really do, if your infection is recent. You might get this test more than once.
- Blood test. These tests, also called interferon-gamma release assays or IGRAs, measure the response when TB proteins are mixed with a small amount of your blood.
If you have a positive skin or blood test, your doctor will probably give you a chest X-ray or CT scan to look for changes in your lungs. They also might test for TB bacteria in your sputum, the mucus that comes up when you cough. These results will help diagnose latent or active TB.
Tuberculosis Treatment
Your treatment will depend on whether you have latent TB or active TB.
- If you have latent TB, your doctor will probably give you medications to kill the bacteria so you don’t develop active TB. If you start to see any of the symptoms of active TB, call your doctor right away.
- Your doctor will treat active TB with a combination of medications. You’ll take them for 6 to 12 months.
Whether you have latent or active TB, it’s important to finish taking all of your medications, even if you feel better after starting them.
Tuberculosis Risks
You can get TB only if you come into contact with others who have it. Other things that could increase your risk include:
- A friend, co-worker, or family member has active TB.
- You live in or have traveled to an area where TB is common, like Russia, Africa, Eastern Europe, Asia, Latin America, and the Caribbean.
- You’re part of a group in which TB is more likely to spread, or you work or live with someone who is. This includes homeless people, people with HIV, people in jail or prison, and people who inject drugs into their veins.
- You work or live in a hospital or nursing home.
- You’re a health care worker for patients at high risk of TB.
- You’re a smoker.Tuberculosis Complications
Tuberculosis Complications
A healthy immune system fights the TB bacteria. But if you have any of the following, you might not be able to fend off active TB disease:
- HIV or AIDS
- Diabetes
- Severe kidney disease
- Head and neck cancers
- Cancer treatments such as chemotherapy
- Low body weight and malnutrition
- Medications for organ transplants
- Certain drugs to treat rheumatoid arthritis, Crohn’s disease, and psoriasis
Babies and young children also are at greater risk because their immune systems aren’t fully formed.
Tuberculosis Prevention
To help stop the spread of TB:
- If you have latent TB, take all of your medication so you don’t develop active TB, which is contagious.
- If you have active TB, limit your contact with other people at work, school, or home. Cover your mouth when you laugh, sneeze, or cough. Wear a surgical mask when you’re around other people during the first weeks of treatment.
- If you’re traveling to a place where TB is common, avoid getting close to or spending a lot of time in crowded places with people who have TB.
Children in countries where TB is common often get the BCG vaccine. It isn’t recommended in the United States. Other vaccines are being developed and tested.
Source: https://www.webmd.com/lung/understanding-tuberculosis-basics#1